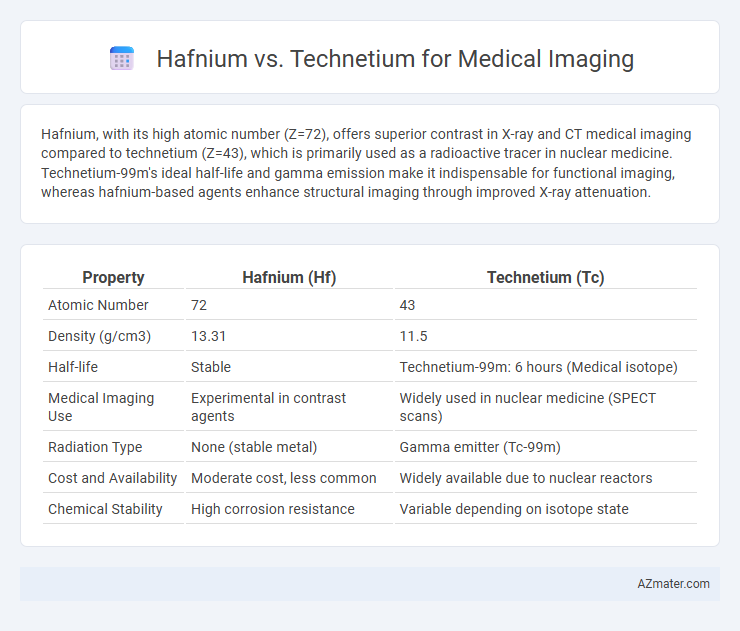
Hafnium, with its high atomic number (Z=72), offers superior contrast in X-ray and CT medical imaging compared to technetium (Z=43), which is primarily used as a radioactive tracer in nuclear medicine. Technetium-99m's ideal half-life and gamma emission make it indispensable for functional imaging, whereas hafnium-based agents enhance structural imaging through improved X-ray attenuation.
Table of Comparison
| Property | Hafnium (Hf) | Technetium (Tc) |
|---|---|---|
| Atomic Number | 72 | 43 |
| Density (g/cm3) | 13.31 | 11.5 |
| Half-life | Stable | Technetium-99m: 6 hours (Medical isotope) |
| Medical Imaging Use | Experimental in contrast agents | Widely used in nuclear medicine (SPECT scans) |
| Radiation Type | None (stable metal) | Gamma emitter (Tc-99m) |
| Cost and Availability | Moderate cost, less common | Widely available due to nuclear reactors |
| Chemical Stability | High corrosion resistance | Variable depending on isotope state |
Overview of Hafnium and Technetium in Medical Imaging
Hafnium and Technetium are elements used in medical imaging due to their unique nuclear properties. Technetium-99m is the most widely used radioisotope in diagnostic imaging, favored for its ideal half-life of six hours and gamma-ray emission suitable for single-photon emission computed tomography (SPECT). Hafnium isotopes, though less common, show potential in therapeutic applications and emerging imaging technologies due to their high atomic number and ability to enhance contrast in advanced imaging modalities.
Chemical Properties Relevant to Imaging Applications
Hafnium exhibits strong X-ray attenuation due to its high atomic number (72) making it suitable for contrast agents in medical imaging, while technetium, with atomic number 43, is prized for its radioactive isotope Tc-99m which emits gamma rays ideal for nuclear imaging. The chemical stability and coordination chemistry of technetium allow for the formation of radiopharmaceuticals that target specific biological sites, enhancing image clarity and specificity. Hafnium's ability to form stable complexes with various ligands complements its potential use in high-resolution computed tomography (CT), whereas technetium's half-life of approximately 6 hours offers optimal imaging times with minimal radiation exposure.
Mechanisms of Action in Diagnostic Procedures
Hafnium-178 generates high-energy photons through isomeric transition, enabling high-resolution imaging in nuclear medicine by targeting specific tissues with minimal radiation exposure. Technetium-99m, the most widely used radioisotope in diagnostic imaging, emits gamma rays detected by gamma cameras, allowing detailed visualization of organ function due to its optimal half-life of six hours and ideal photon energy of 140 keV. The mechanism of action for technetium involves binding with various radiopharmaceutical compounds, facilitating precise molecular targeting and real-time assessment of physiological processes.
Advantages of Technetium-Based Radiopharmaceuticals
Technetium-99m is the most widely used radioisotope in nuclear medicine due to its ideal physical half-life of six hours and gamma-ray emission of 140 keV, which ensures high-quality imaging with minimal radiation dose to patients. Its versatile chemistry allows for easy labeling of a wide range of biologically active molecules, enabling targeted imaging of different organs and pathological conditions. In contrast, hafnium isotopes lack the well-established radiopharmaceutical frameworks and optimized emission properties that make technetium-99m indispensable in diagnostic imaging.
Emerging Uses of Hafnium Compounds in Imaging
Hafnium compounds, particularly hafnium oxide nanoparticles, are gaining traction in medical imaging due to their high atomic number and strong X-ray attenuation properties, which enhance contrast in computed tomography (CT) scans. Unlike technetium-99m, the traditional radionuclide used in nuclear medicine imaging, hafnium-based agents offer promising biocompatibility and reduced radiation dose. Emerging research highlights hafnium's potential in theranostics, combining diagnostic imaging and targeted radiotherapy, positioning it as a versatile alternative in advanced medical diagnostics.
Safety Profiles and Toxicity Comparisons
Hafnium and Technetium are both used in medical imaging, but Technetium-99m is the most widely employed radioisotope due to its ideal half-life and gamma emission suitable for diagnostic scans. Hafnium's radioisotopes are less common and have limited data on their safety profile, though preliminary studies suggest relatively low toxicity compared to heavier metals. Technetium-99m demonstrates a well-documented safety profile with minimal adverse effects, whereas Hafnium requires further research to fully establish its toxicity and biocompatibility for clinical use.
Radiological Imaging Performance: Hafnium vs Technetium
Hafnium and Technetium exhibit distinct radiological imaging performance due to their differing nuclear properties and isotopes. Technetium-99m remains the gold standard in medical imaging for its ideal half-life of 6 hours and gamma emission energy of 140 keV, providing high-resolution images with minimal radiation dose. Hafnium isotopes, while explored for their potential neutron capture properties, lack the optimal gamma emission characteristics and established radiopharmaceutical applications found in Technetium, limiting their current utility in diagnostic radiology.
Availability and Cost-Effectiveness
Technetium-99m is widely favored in medical imaging due to its optimal availability from molybdenum-99 generators and relatively low production cost, making it a cost-effective choice for diagnostic procedures. Hafnium isotopes, while having potential imaging properties, are less accessible because they require specialized production methods, leading to higher costs and limited clinical application. The established supply chain and economic efficiency of technetium-99m solidify its dominance in nuclear medicine over hafnium-based alternatives.
Future Research and Innovations in Imaging Agents
Hafnium and technetium exhibit unique properties that influence their potential in medical imaging, with technetium-99m currently dominating nuclear medicine due to its ideal half-life and gamma emission. Future research aims to enhance hafnium-based agents by leveraging its strong neutron-capture capabilities for advanced radiotherapy combined with imaging, known as theranostics. Innovations focus on developing hafnium nanoparticles conjugated with targeting ligands to improve specificity and reduce toxicity, while technetium derivatives continue to be optimized for higher resolution and multi-modal imaging applications.
Clinical Recommendations and Practical Considerations
Technetium-99m remains the gold standard for medical imaging due to its ideal half-life (6 hours) and gamma emission, providing high-resolution images with minimal radiation exposure. Hafnium isotopes, while under investigation for theranostic applications, currently lack extensive clinical validation and widely accepted protocols, limiting their routine use in diagnostic imaging. Practical considerations favor technetium-99m, including established production infrastructure, well-documented safety profiles, and broader availability for nuclear medicine procedures.
Infographic: Hafnium vs Technetium for Medical Imaging
 azmater.com
azmater.com