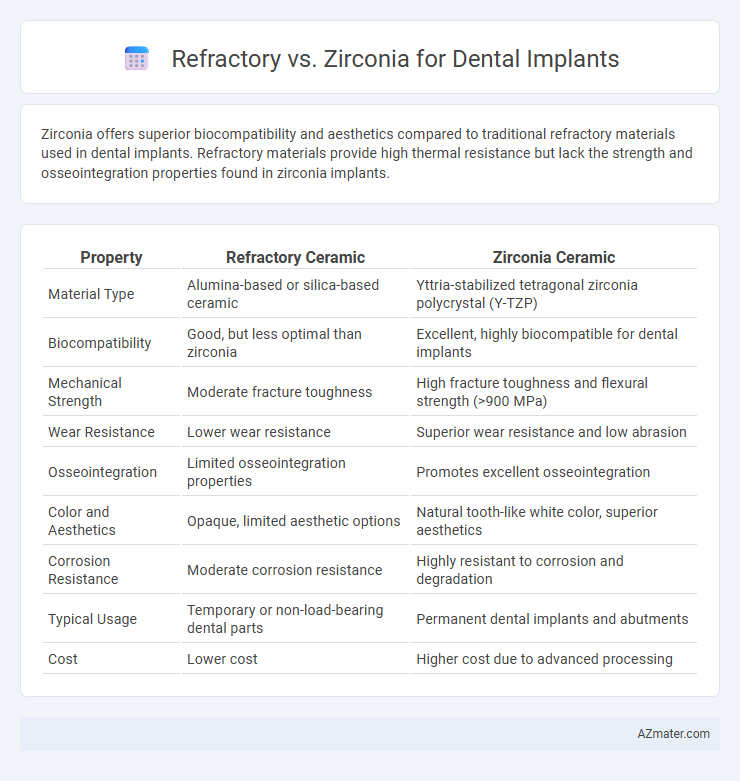
Zirconia offers superior biocompatibility and aesthetics compared to traditional refractory materials used in dental implants. Refractory materials provide high thermal resistance but lack the strength and osseointegration properties found in zirconia implants.
Table of Comparison
| Property | Refractory Ceramic | Zirconia Ceramic |
|---|---|---|
| Material Type | Alumina-based or silica-based ceramic | Yttria-stabilized tetragonal zirconia polycrystal (Y-TZP) |
| Biocompatibility | Good, but less optimal than zirconia | Excellent, highly biocompatible for dental implants |
| Mechanical Strength | Moderate fracture toughness | High fracture toughness and flexural strength (>900 MPa) |
| Wear Resistance | Lower wear resistance | Superior wear resistance and low abrasion |
| Osseointegration | Limited osseointegration properties | Promotes excellent osseointegration |
| Color and Aesthetics | Opaque, limited aesthetic options | Natural tooth-like white color, superior aesthetics |
| Corrosion Resistance | Moderate corrosion resistance | Highly resistant to corrosion and degradation |
| Typical Usage | Temporary or non-load-bearing dental parts | Permanent dental implants and abutments |
| Cost | Lower cost | Higher cost due to advanced processing |
Introduction to Dental Implant Materials
Dental implant materials must exhibit biocompatibility, strength, and durability to ensure successful osseointegration and long-term function. Refractory materials, such as alumina and magnesium oxide-based ceramics, provide high thermal resistance and mechanical stability but may lack the translucency needed for optimal esthetics. Zirconia, a high-performance ceramic, offers superior fracture toughness, excellent biocompatibility, and natural tooth-like appearance, making it increasingly preferred for dental implant abutments and crowns.
Understanding Refractory Materials in Dentistry
Refractory materials, known for their high thermal stability and resistance to deformation, play a crucial role in dental implant fabrication by providing a stable mold environment during the casting process. Zirconia, a type of advanced ceramic refractory material, offers exceptional biocompatibility, strength, and aesthetic qualities, making it a preferred choice for permanent dental implants over traditional metal-based refractory materials. Understanding the thermal behavior, mechanical properties, and biocompatibility of these refractory materials ensures optimal implant fit, durability, and patient outcomes in restorative dentistry.
What is Zirconia? Key Properties and Advantages
Zirconia, a high-performance ceramic material composed of zirconium dioxide, is increasingly favored in dental implants for its exceptional biocompatibility and strength. Its key properties include high fracture toughness, corrosion resistance, and excellent aesthetic qualities due to its tooth-like color. Zirconia's advantages in dental applications involve reduced risk of allergic reactions, superior osseointegration, and minimal plaque accumulation compared to traditional refractory metals.
Comparing Biocompatibility: Refractory vs Zirconia
Refractory materials in dental implants exhibit moderate biocompatibility but may trigger inflammatory responses due to their metallic composition. Zirconia demonstrates superior biocompatibility with high resistance to corrosion and reduced plaque accumulation, promoting better soft tissue integration. Clinical studies show zirconia implants have lower incidences of peri-implantitis compared to refractory alloys, making them preferable for patients with metal sensitivities.
Mechanical Strength and Durability Differences
Refractory materials for dental implants offer excellent thermal resistance but generally provide lower mechanical strength compared to zirconia, which is known for its superior fracture toughness and high flexural strength exceeding 900 MPa. Zirconia's durability is enhanced by its ability to resist wear and crack propagation, making it a preferred choice for long-term dental implant applications. In contrast, refractory materials may require additional surface treatments or reinforcements to match the longevity and mechanical resilience inherent in zirconia implants.
Aesthetic Outcomes: Shade and Translucency
Zirconia offers superior aesthetic outcomes for dental implants due to its natural tooth-like shade and translucency, closely mimicking the appearance of enamel. Refractory materials typically lack the translucency of zirconia, resulting in a less lifelike appearance and a higher risk of greyish discoloration under thin gingival tissue. Optimizing the choice between refractory and zirconia depends heavily on the desired shade matching and translucency for optimal aesthetic integration in the patient's smile.
Clinical Performance and Longevity
Refractory materials and zirconia differ in clinical performance and longevity for dental implants, with zirconia offering superior biocompatibility and resistance to fracture, promoting better osseointegration and long-term stability. Clinical studies demonstrate zirconia's lower plaque accumulation and enhanced aesthetic outcomes compared to refractory materials, which may exhibit higher wear and susceptibility to chipping over time. Zirconia implants provide durable performance with reduced risk of peri-implantitis, contributing to extended implant lifespan and patient satisfaction.
Cost Comparison: Refractory vs Zirconia Implants
Refractory implants generally cost less than zirconia implants due to lower material and manufacturing expenses, making them a more budget-friendly option for dental restoration. Zirconia implants, while more expensive, offer superior biocompatibility and aesthetics, which may justify the higher investment for patients seeking metal-free solutions. Cost differences can vary depending on the dental lab, geographic location, and specific implant system used, but refractory options typically fall within a more affordable price range.
Indications and Contraindications for Each Material
Refractory ceramics are indicated for dental implant frameworks requiring high thermal stability and resistance to deformation during porcelain firing, making them suitable for metal-ceramic restorations but contraindicated in esthetically demanding anterior regions due to limited translucency. Zirconia is favored for implants needing high fracture strength and superior esthetics, especially in anterior restorations and patients with metal allergies, but contraindicated in cases with bruxism or insufficient occlusal clearance due to its brittleness and risk of fracture. Selecting between refractory ceramics and zirconia depends on balancing mechanical demands, esthetic requirements, and patient-specific factors such as occlusion and biocompatibility.
Choosing the Right Material for Dental Implant Success
Refractory ceramics provide high thermal stability and resistance to corrosion, making them suitable for enduring the stresses of dental implant procedures, while zirconia offers superior biocompatibility and esthetic advantages due to its tooth-like color and strength. Selecting the right material for dental implant success depends on factors like patient-specific biological response, mechanical load requirements, and aesthetic preferences. Studies show zirconia implants reduce inflammation risks and promote osseointegration, whereas refractory ceramics excel in durability under extreme conditions.
Infographic: Refractory vs Zirconia for Dental Implant
 azmater.com
azmater.com